
There was no postoperative infarction (0%). Pipeline embolization was performed in 2 patients, including 1 (50%) who had recurrence. Vertebral artery trapping with vertebral artery-posterior inferior cerebellar artery stenting was performed in 4 patients, including 1 (25%) who had postoperative cerebellar infarction. Stent-assisted coil embolization was performed in 8 patients, including 1 (12.5%) who had postoperative cerebellar infarction and 2 (25%) who had recurrence. Multiple stenting was performed in 4 patients, including 1 (25%) who had cerebellar infarction and 1 (25%) who had recurrence. Subarachnoid hemorrhage was diagnosed initially in 6 of 18 patients, and infarction was diagnosed initially in 2 patients. Clinical and radiologic information were obtained from retrospective chart review and radiologic review. Treatments were multiple stenting, stent-assisted coil embolization, vertebral artery trapping with vertebral artery-posterior inferior cerebellar artery stenting, and Pipeline embolization.
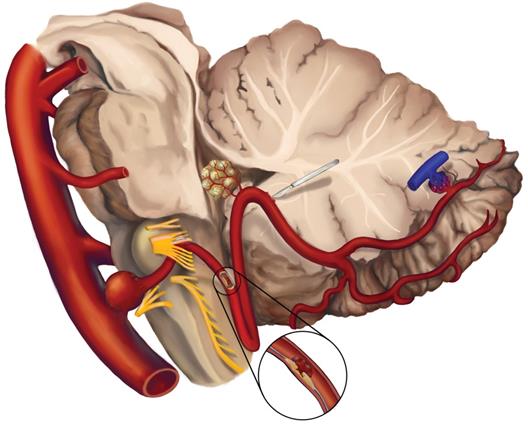
This study included 18 vertebral artery dissecting aneurysms (6 ruptured and 12 unruptured) involving posterior inferior cerebellar artery treated from January 2009 to December 2016. No commercial use is permitted unless otherwise expressly granted.To determine clinical and radiologic outcomes of vertebral artery dissecting aneurysms involving posterior inferior cerebellar artery according to different types of endovascular treatment. © Article author(s) (or their employer(s) unless otherwise stated in the text of the article) 2018. The proposed classification system aids in that selection.Īnastomosis aneurysm bypass flow diversion pipeline embolization device posterior inferior cerebellar artery vertebral artery. We present the first described cases of successful PED treatment of PICA aneurysms with direct placement of the PED in the PICA vessel itself. The PED may be used successfully to treat select aneurysms of the PICA. All PEDs were patent and all patients were independent at the last follow-up. Three patients had the PED placed entirely in the PICA and no patient suffered from a medullary or cerebellar stroke. All aneurysms were successfully treated, with 8/10 completely obliterated and 2 with a partial reduction in size. These were classified based on their morphology and location into two main types and five total subtypes for consideration of treatment with flow diversion. Vertebral aneurysms without disease in the PICA were excluded from the study.ġ0 PICA aneurysms were treated during the study period. PICA aneurysms were defined as aneurysms that involved the PICA. Patient and aneurysm data as well as angiographic imaging were reviewed for all cases of PICA aneurysms treated with the PED. Institutional databases of neuroendovascular procedures were reviewed for cases of intracranial aneurysms treated with the PED. We assessed our multi-institutional experience treating these lesions, including the first reported cases of the PED placed within the PICA. Due to the unique anatomy and morphology of these aneurysms, it requires special attention. While there are reports of treating PICA aneurysms using placement of FD stents in the vertebral artery, there are no reports of treating these lesions by placement of flow diverting stents in the PICA vessel itself.
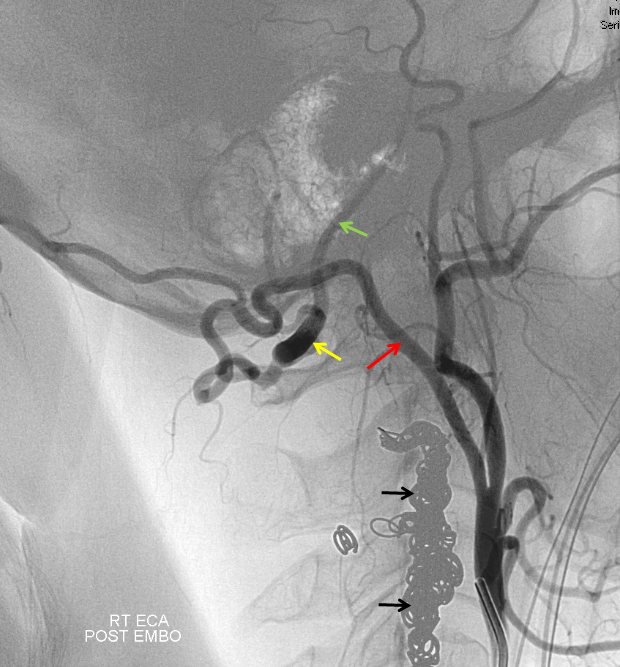
However, treatment of posterior inferior cerebellar artery (PICA) aneurysms with flow diversion (FD) has not been specifically described or discussed. The pipeline embolization device (PED) is frequently used in the treatment of anterior circulation aneurysms, especially around the carotid siphon, with generally excellent results.


 0 kommentar(er)
0 kommentar(er)
